In May, I went for a consultation with Dr Linskey at UC Irvine Medical Center in CA. He said that he could see vascular contact with my trigeminal nerve and that I was a candidate for MVD surgery, despite being told otherwise by 2 neurosurgeons and various other Drs here in UT. Two weeks later, we made the decision to move forward with surgery and scheduled for July 21. I had a lumbar puncture to rule out MS, which was clear. And this past week I had blood work, chest xray and EKG.
We have had an online fundraiser to help with the costs and we have been overwhelmed with gratitude for the generosity of so many friends and family. It's been amazing. We have to arrive in CA for pre op appts 2 days before surgery. Then the neurosurgeon requires that we stay in the area, not more than 20-30 min away from the hospital, for 14-15 days post op in case of complications and to have follow up visits. This means we will be in CA for about 2 1/2 weeks total. Then we will probably need to travel again to CA for follow ups at 3 months, 6 months, a year and possibly every year thereafter (I'm not positive on that.) So, there are a lot of costs. We are thankful to have insurance though, which means we will only have to meet the $7000 out of pocket maximum. For a surgery that runs close to $150,000 in total cost, this is a huge blessing.
Anyway, I've had a lot of people ask me questions and I imagine a lot of questions are being thought but unasked, so I thought I'd address most of the ones I can think of in a blog post. Hopefully this covers most everything.
1. What is an MVD? What will they do?
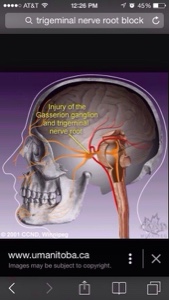
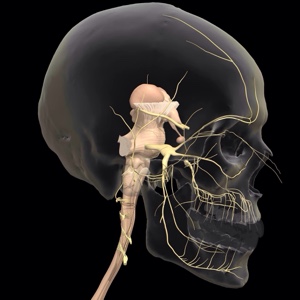
MVD stands for microvascular decompression. The neuralgia is being caused by blood vessels compressing, rubbing, or pressing on the cranial nerves (in my case he will look at 4 cranial nerves, #5, 7, 9 and 10). The surgery will remove a small section of skull behind my ear, they go in and look at the nerves near where they are exiting the brain stem and remove any blood vessels away from the nerves. They pad the arteries from the nerves with teflon padding. The veins are cut away and cauterized. They then replace the piece of skull with "bone cement" and stitch everything back up.
2. Why do you need an MVD? Aren't there less invasive surgeries or treatments for trigeminal neuralgia?
TN is a progressive disease. The longer the blood vessels rub against the nerves, the more damage is done over time. Because of this, experts in TN say that MVD's are most effective if done in the first 7 years since onset of symptoms. I'm already 4 years in. I have tried over 30 medications, and also done other procedures which haven't helped. There are less invasive surgeries but they work by damaging the nerve to prevent it from sending pain signals. They do not remove the cause of the pain, the blood vessels. And so the nerve heals itself over time and symptoms are likely to recur. Plus I had other neurosurgeons tell me I wasn't a candidate for any of those surgeries anyway. Then after you damage the nerve in these surgeries, if you then decide to try an MVD later, it is less likely to be successful due to all the additional damage done to the nerve. If there are compressions on the nerve, an MVD is the only procedure that removes the cause of the pain.
3. Will you be pain free after this surgery? Will you be fixed, all better?
This is the clincher. Even though MVD removes the vessels from compressing the nerve, it is still not always successful. It is very individual. Sometimes the nerve just doesn't heal well from all of the damage from the compression. Sometimes there are complications which make things even worse after the surgery. Sometimes the veins that were cut (if there were any) grow back and the pain returns. Sometimes the teflon shifts and the artery comes in contact with the nerve again. I don't even know all what might happen. It just doesn't always work. There are also 2 types of pain with TN: the episodic shocks of pain, and the constant aching pain. Not everyone has both types, but I do. The surgeon says there is an 80% chance of resolving the episodic shocks. But only a 50% chance of a 50% reduction in the constant pain. And then, in my case, I also have the chronic migraines, and he doesn't think they are related to the TN and surgery is not likely to have any effect on them. So. Even best case scenario with these chances of success, I will not be pain free. Almost guaranteed. And worse case scenario is just too scary to think about right now.... But that is the reality we are faced with.
4. So why are you even doing this risky, complicated brain surgery with an open craniotomy and the chance of complications, and a definite long recovery if you don't even know if it will work?
The million dollar question. The simplest answer I come back to again and again when I ask myself this question is this:
I don't know what else to do.
I have to try.
I don't know what else to do.
Because I can't keep going with no help.
I have to try.
Because I'll never know unless I do.
Also I remind myself that TN is a progressive disorder and will only get worse over time. I have a 7 yr window where the likliehood of success of this procedure is the best, so if I'm ever going to do it, now seems like a better time than just waiting. It just seems to be a step that I need to do, even if it only results in a reduction in some of my pain. Who knows how that might be for me? There is no way to know. It may not be any better for me, in terms of functionality or outlook, but it might help....
Also I feel like I should add that we have fasted and prayed a lot about this decision and, although I have not yet received the positive confirmation in the way *I would have liked*, my strongest impression is that this is a necessary step. I don't know for sure that this will be successful for me, but I just know it's something I need to do. So we move forward, step by step, taking one piece at a time, in the way that feels right. It's all we can do.
5. What is the recovery like?
Full recovery takes 12-18 months. I will have activity restrictions until I get cleared at 1 year. They don't want you to risk hitting your head or anything like that. Other than that, it depends on how the recovery goes, but it is definitely a long painful road of recovery. Dizziness, headaches, and nausea are very common for weeks. Most people say it takes at least a couple months before they are able to do very much. If there are complications, then of course recovery is even more . . . complicated. Numbness in the face and scalp is common. Sometimes there is some paralysis as the nerve heals. Recovery and possible complications are scary. Mostly because it's just so unknown. It's kind of like childbirth, you can hear all the stories, the good, the bad, the dreamy ones, the nightmare ones, but when it comes down to it, you really have no idea - AT ALL - what it will be like for you. You just have to do it. I am equally freaked out by the really easy recoveries I hear some people have, as I am the scary stories I hear about the really hard parts. Because guess what?! None of them is me. I would rather know everything I can and be prepared for the worst. But that's just me.
6. Why do you have to go to CA for this? Aren't there surgeons who do it in UT?
There are surgeons who perform this in UT, but from my own experience and from what I've heard, most will only do it on patients who only have the stabbing shock type of pain and who have clear compressions visible on MRI (Drs here said I didn't have compressions, even though Dr L said he could see them) - at any rate, I was not deemed a candidate for surgery. Also, although Dr L was very adamant in reminding us that he is not the only surgeon qualified to do this, he did give us some qualifications we should look for in a surgeon to do this. A few that stand out to me are that they should be members of the Trigeminal Neuralgia Association (there aren't any in UT), they should have been trained directly under Dr Janetta who pioneered the procedure (none in UT), and they should perform at least 5 MVD's a year, which is hard to find (he does about 50). He even said himself that he doesn't know any surgeons who meet this criteria in UT. So, if I would have to travel anyway to find a highly qualified neurosurgeon, I figure I might as well travel to one that I know is one of the top experts in the field of TN, and who has performed this surgery on other people I know personally.
7. So how do you feel about all this? Are you excited, nervous, freaked out?
Here's the thing. When the words Trigeminal Neuralgia were first brought up to me in Aug of 2011, I started researching whatever I could find. I quickly bought the book Striking Back, which is published by the National Facial Pain Association and is kind of considered the TN bible. I read about all the common medication treatments and available surgeries and treatments. I think I have always known that if MVD were a possibility for me, I would do it. But I had 2 neurosurgeons and 3 neurologists tell me I wasn't a candidate for any surgery. I gave up on it. It was over a year ago that I started hearing about Dr Linskey, other people's good experiences with him. I knew he was on the board of the Trigeminal Neuralgia Association and that he helped some patients who weren't helped by anyone else. And at one time, over a year ago, I actually had someone offer to help pay for the costs to get me to CA to see him. So I thought about it a lot then. We had different insurance then that didn't cover any out of state Drs, so it wasn't really a possibility. Then I had a year of breast issues that culminated in surgery this year (still having some pain from that surgery), which took precedence over looking into this further. But then we were able to change insurances April 1 this year. The person who had offered help was no longer in a position to do so, but it was his offer that had started the process of thinking through what I might do, if given the opportunity.
So, here I am.
I am scared, nervous and unsure if I am doing the right thing. It's hard for me to talk about. There are so many components. Getting through the surgery itself (lots of risks), possible post op complications, dealing with a normal recovery, wondering if it will work, and how soon I will know if it worked, worrying about leaving my kids in the care of someone else for nearly 3 weeks, worrying about how much they might be worrying about me and this surgery, all of the logistics: making sure the kids have ways to get where they need to be, needs taken care of, travel and lodging for me and Zac, Zac working while we are staying there, financial concerns, longer term post op worries, worrying about letting people down (even though I know I shouldn't, it's still there), people who have contributed to our fundraiser to help make this even possible, wanting this to be a successful, miraculous story, wanting or wishing to be "inspirational" - whatever that means - I feel a lot of pressure in it all, but just feeling too much like I am a failure in all of it, not knowing if I am strong enough to handle any of this, and do I have enough faith or any at all. So much of it I can't sort out in my head, and I don't have the answers or know even where to start. I don't even know if all of that begins to scratch the surface. But that is some of what goes through my head when someone asks how I feel.
Well, this post has probably gone on far too long anyway. But I hope this answers some of the questions some of you might have. Feel free to ask anything else you'd like and I will try my best to answer. Words of encouragement, love and support as well as prayers and good thoughts are always always welcome. Thank you again for reading and being there for me through all of this.
And a HUGE thank you to everyone that has helped out with financial contributions. Every little bit helps in relieving some of the burden and we are so grateful. Thank you.
5. What is the recovery like?
Full recovery takes 12-18 months. I will have activity restrictions until I get cleared at 1 year. They don't want you to risk hitting your head or anything like that. Other than that, it depends on how the recovery goes, but it is definitely a long painful road of recovery. Dizziness, headaches, and nausea are very common for weeks. Most people say it takes at least a couple months before they are able to do very much. If there are complications, then of course recovery is even more . . . complicated. Numbness in the face and scalp is common. Sometimes there is some paralysis as the nerve heals. Recovery and possible complications are scary. Mostly because it's just so unknown. It's kind of like childbirth, you can hear all the stories, the good, the bad, the dreamy ones, the nightmare ones, but when it comes down to it, you really have no idea - AT ALL - what it will be like for you. You just have to do it. I am equally freaked out by the really easy recoveries I hear some people have, as I am the scary stories I hear about the really hard parts. Because guess what?! None of them is me. I would rather know everything I can and be prepared for the worst. But that's just me.
6. Why do you have to go to CA for this? Aren't there surgeons who do it in UT?
There are surgeons who perform this in UT, but from my own experience and from what I've heard, most will only do it on patients who only have the stabbing shock type of pain and who have clear compressions visible on MRI (Drs here said I didn't have compressions, even though Dr L said he could see them) - at any rate, I was not deemed a candidate for surgery. Also, although Dr L was very adamant in reminding us that he is not the only surgeon qualified to do this, he did give us some qualifications we should look for in a surgeon to do this. A few that stand out to me are that they should be members of the Trigeminal Neuralgia Association (there aren't any in UT), they should have been trained directly under Dr Janetta who pioneered the procedure (none in UT), and they should perform at least 5 MVD's a year, which is hard to find (he does about 50). He even said himself that he doesn't know any surgeons who meet this criteria in UT. So, if I would have to travel anyway to find a highly qualified neurosurgeon, I figure I might as well travel to one that I know is one of the top experts in the field of TN, and who has performed this surgery on other people I know personally.
7. So how do you feel about all this? Are you excited, nervous, freaked out?
Here's the thing. When the words Trigeminal Neuralgia were first brought up to me in Aug of 2011, I started researching whatever I could find. I quickly bought the book Striking Back, which is published by the National Facial Pain Association and is kind of considered the TN bible. I read about all the common medication treatments and available surgeries and treatments. I think I have always known that if MVD were a possibility for me, I would do it. But I had 2 neurosurgeons and 3 neurologists tell me I wasn't a candidate for any surgery. I gave up on it. It was over a year ago that I started hearing about Dr Linskey, other people's good experiences with him. I knew he was on the board of the Trigeminal Neuralgia Association and that he helped some patients who weren't helped by anyone else. And at one time, over a year ago, I actually had someone offer to help pay for the costs to get me to CA to see him. So I thought about it a lot then. We had different insurance then that didn't cover any out of state Drs, so it wasn't really a possibility. Then I had a year of breast issues that culminated in surgery this year (still having some pain from that surgery), which took precedence over looking into this further. But then we were able to change insurances April 1 this year. The person who had offered help was no longer in a position to do so, but it was his offer that had started the process of thinking through what I might do, if given the opportunity.
So, here I am.
I am scared, nervous and unsure if I am doing the right thing. It's hard for me to talk about. There are so many components. Getting through the surgery itself (lots of risks), possible post op complications, dealing with a normal recovery, wondering if it will work, and how soon I will know if it worked, worrying about leaving my kids in the care of someone else for nearly 3 weeks, worrying about how much they might be worrying about me and this surgery, all of the logistics: making sure the kids have ways to get where they need to be, needs taken care of, travel and lodging for me and Zac, Zac working while we are staying there, financial concerns, longer term post op worries, worrying about letting people down (even though I know I shouldn't, it's still there), people who have contributed to our fundraiser to help make this even possible, wanting this to be a successful, miraculous story, wanting or wishing to be "inspirational" - whatever that means - I feel a lot of pressure in it all, but just feeling too much like I am a failure in all of it, not knowing if I am strong enough to handle any of this, and do I have enough faith or any at all. So much of it I can't sort out in my head, and I don't have the answers or know even where to start. I don't even know if all of that begins to scratch the surface. But that is some of what goes through my head when someone asks how I feel.
Well, this post has probably gone on far too long anyway. But I hope this answers some of the questions some of you might have. Feel free to ask anything else you'd like and I will try my best to answer. Words of encouragement, love and support as well as prayers and good thoughts are always always welcome. Thank you again for reading and being there for me through all of this.
And a HUGE thank you to everyone that has helped out with financial contributions. Every little bit helps in relieving some of the burden and we are so grateful. Thank you.
Some pictures and illustrations:
This is what the incision will look like: